Pressure Injuries
Pressure injuries, also called bedsores or pressure ulcers, are among the most preventable yet challenging wounds in healthcare. They develop when prolonged pressure restricts blood flow to the skin and underlying tissues, causing damage that ranges from surface redness to deep wounds exposing muscle or bone. For patients with limited mobility—whether recovering from surgery, managing chronic illness, or requiring long-term care—pressure injuries pose a serious threat to health, comfort, and quality of life.
At Best Wound Care, we understand that pressure injuries require more than basic wound dressings. They demand expert assessment, specialized treatment protocols, and proactive prevention strategies to heal existing wounds and stop new ones from forming.
Our Approach to Pressure Injuries
We utilize evidence-based treatments tailored to each wound's characteristics.
Expert Assessment Our Nurse Practitioners conduct thorough evaluations to determine pressure injury stage, assess tissue viability, identify contributing factors, and develop individualized treatment plans. Accurate staging guides treatment selection and sets realistic healing expectations.
Debridement
to remove non-viable tissue and promote healthy granulation
Antimicrobial therapies
when infection is present or suspected
Moisture-balancing dressings
that protect the wound while managing drainage
Advanced biologic therapies
for complex or non-healing pressure injuries
Understanding Pressure Injuries
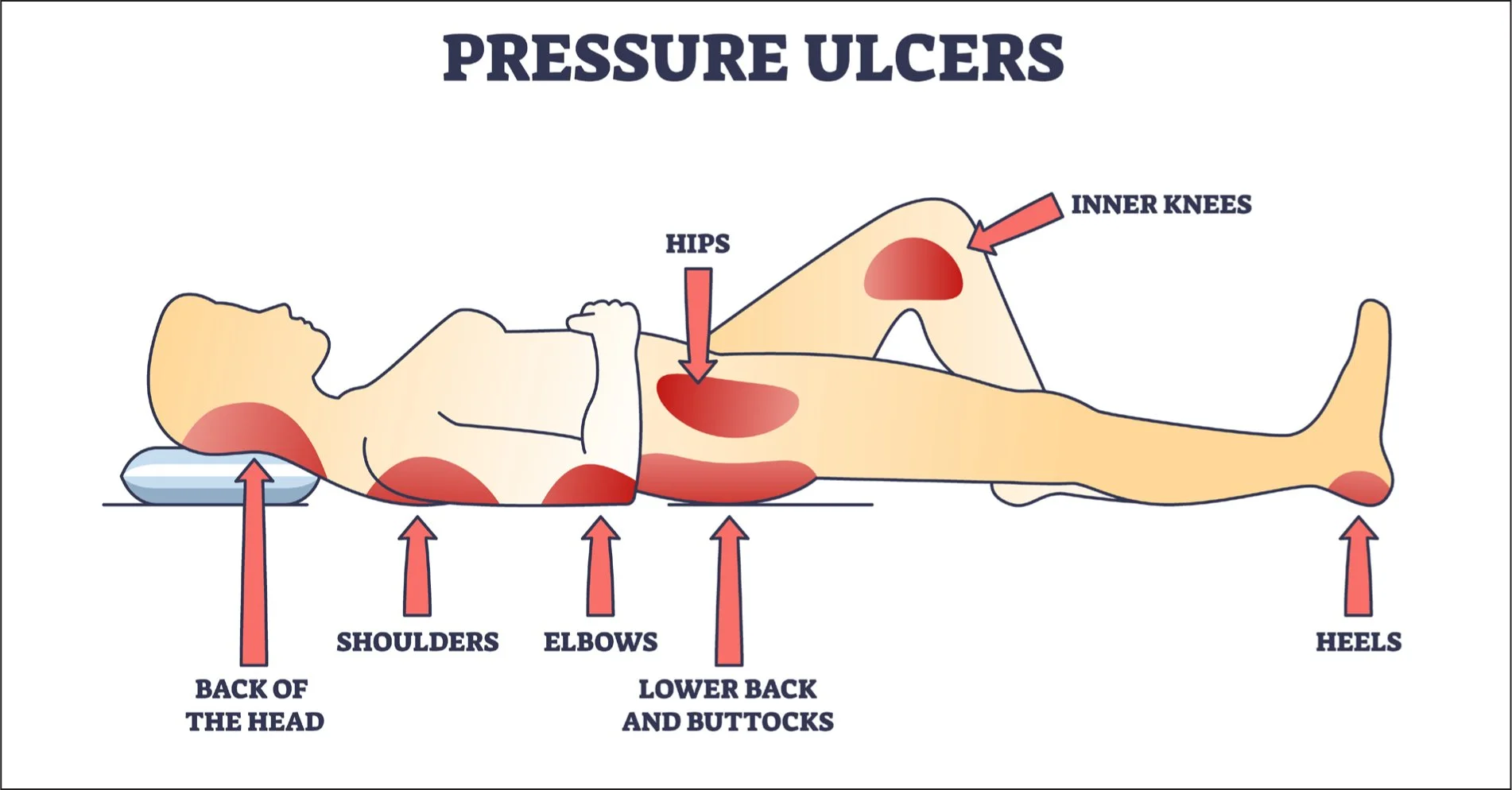
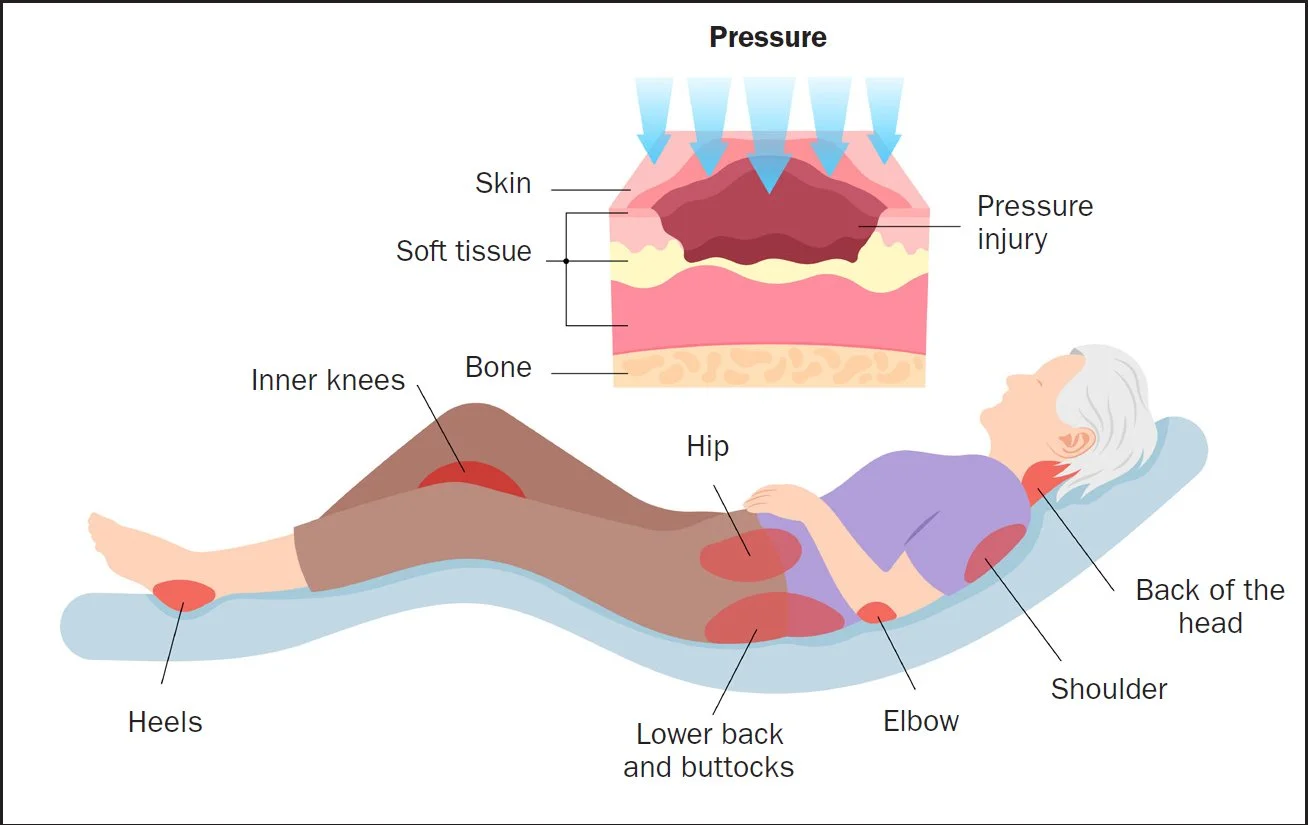
Pressure injuries occur when sustained pressure—often combined with friction or shear forces—damages skin and tissue. Common sites include areas where bone is close to the skin surface: the tailbone, hips, heels, elbows, and shoulder blades.
Key Contributing Factors:
Immobility – Patients who cannot reposition themselves independently face the highest risk
Moisture – Incontinence, perspiration, or wound drainage weakens skin integrity
Poor Nutrition – Inadequate protein and nutrients impair the body's ability to maintain healthy tissue
Medical Conditions – Diabetes, vascular disease, and neurological conditions increase vulnerability
Friction and Shear – Sliding against sheets or being pulled during transfers damages delicate skin
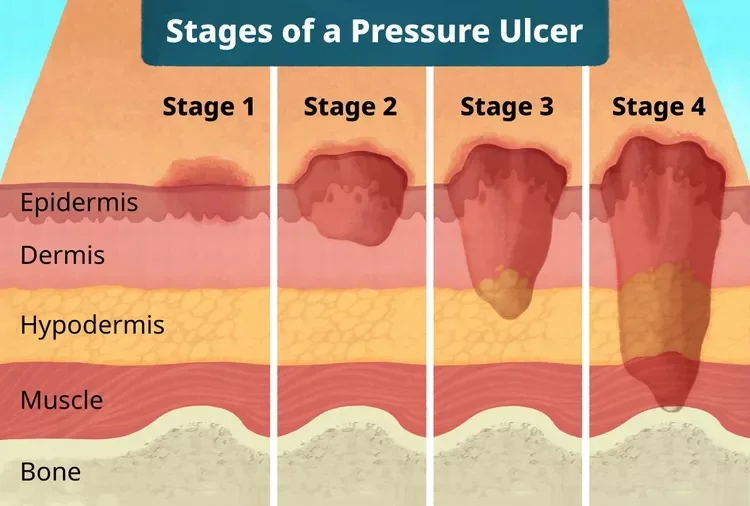
Pressure injuries progress through stages, from Stage I with intact skin showing redness to Stage IV with full-thickness tissue loss with exposed bone or muscle. Deep tissue injuries and unstageable wounds (obscured by eschar or slough) present additional complexity.
What Successful Healing Looks Like
Success means not just closing the current wound, but preventing recurrence through ongoing risk assessment and prevention strategies.
Throughout treatment, our Nurse Practitioners monitor progress through:
Regular wound measurements tracking size reduction
Tissue quality improvement (healthy granulation replacing necrotic tissue)
Decreased drainage and odor
Wound edge advancement toward closure
Reduced pain and increased patient comfort
‘
Healing timelines for pressure injuries vary based on wound severity, patient health, and adherence to pressure relief:
Stage 1-2 Pressure Injuries may heal within 2-6 weeks with care and consistent pressure relief
Stage 3 Pressure Injuries typically require 1-4 months of specialized treatment
Stage 4 Pressure Injuries often need 3-6 months or longer, and may require surgical intervention
Signs You Need Specialized Care
Certain signs indicate a pressure injury requires expert intervention beyond basic wound care:
Wounds that haven't improved after 2 weeks of treatment
Increasing wound size despite appropriate care
Foul odor, increased drainage, or signs of infection
Exposed bone, tendon, or muscle (Stage IV)
Multiple pressure injuries in one patient
Patient experiencing significant pain
If any of these conditions are present, specialized wound care can prevent complications and accelerate healing.
Contact us
Pressure injuries don't have to derail recovery or diminish quality of life. With expert assessment, specialized treatment, and comprehensive prevention strategies, our Nurse Practitioners provide the care your patients need to heal and stay healthy.
Contact Best Wound Care today to bring specialized pressure injury expertise to your facility.