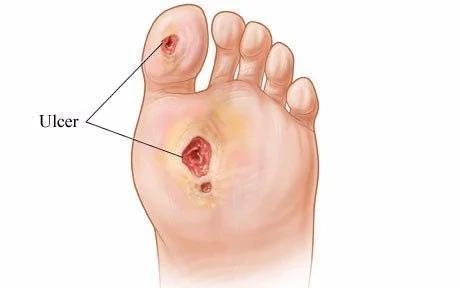
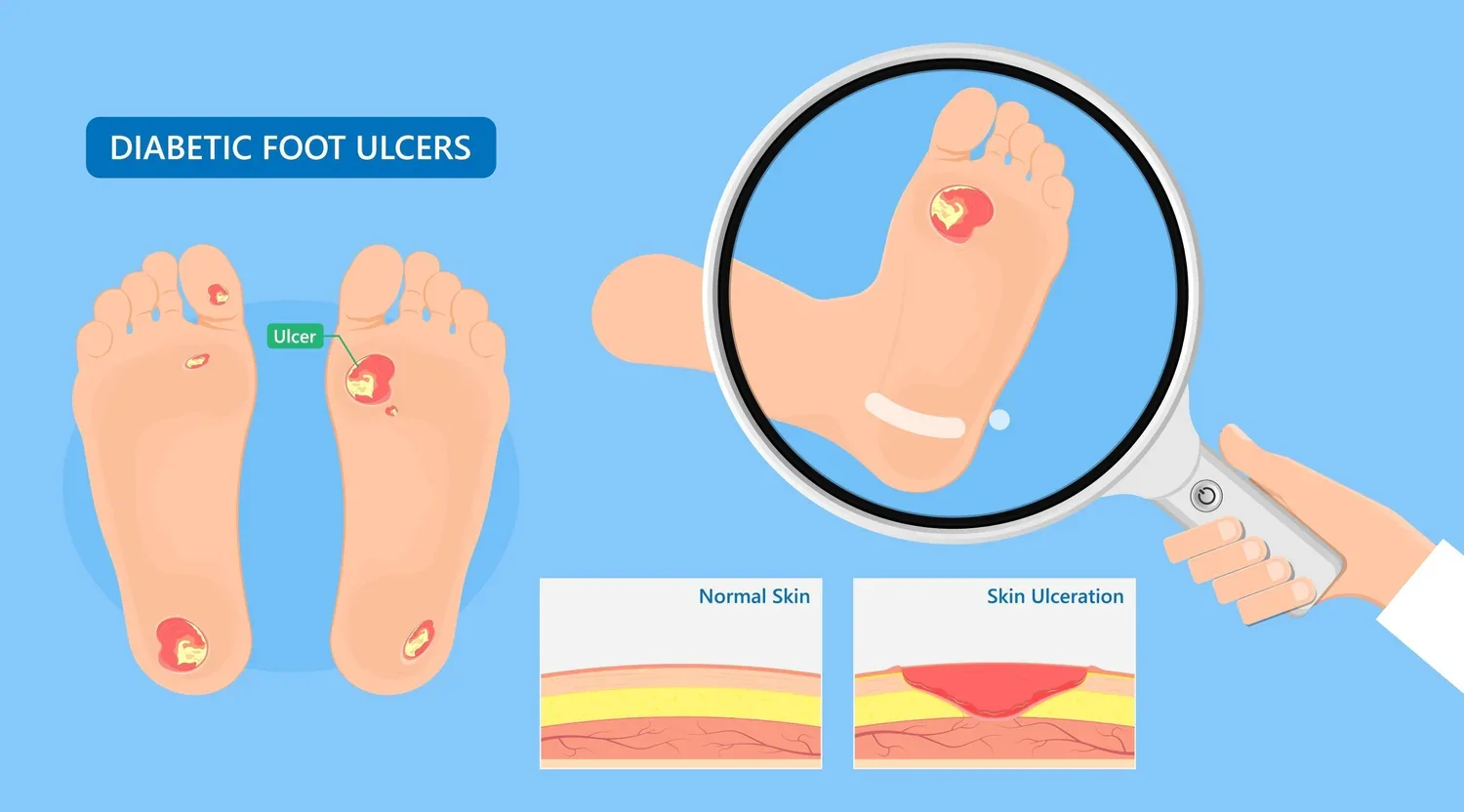
Diabetic Foot Ulcers
Diabetic foot ulcers are one of the most serious complications of diabetes, affecting approximately 15% of people with diabetes during their lifetime. These open sores most commonly develop on the bottom of the foot and can quickly progress from a minor wound to a limb-threatening condition. Left untreated or improperly managed, diabetic foot ulcers can lead to severe infection, hospitalization, and amputation.
At Best Wound Care, we specialize in the complex treatment diabetic foot ulcers require. Our Nurse Practitioners understand that successful healing demands more than wound dressings—it requires addressing the unique challenges diabetes creates, from impaired circulation to diminished sensation that allows injuries to go unnoticed.
Understanding Diabetic Foot Ulcers
Diabetic foot ulcers result from a dangerous combination of factors that diabetes creates:
Nerve Damage
High blood sugar levels over time damage nerves in the feet, causing loss of protective sensation. Patients cannot feel pressure, heat, or pain that would normally warn of injury. A small blister, cut, or area of pressure can progress to a serious ulcer without the patient realizing anything is wrong.
Foot Deformities
Diabetes can cause changes in foot structure—hammertoes, bunions, Charcot foot—that create abnormal pressure points. These high-pressure areas are where ulcers most commonly form. Common ulcer locations include the ball of the foot, tips of toes, bottom of the big toe, between toes, and the heel
Poor Circulation
Diabetes damages blood vessels, reducing blood flow to the feet and lower legs. Inadequate circulation means wounds receive less oxygen and fewer nutrients needed for healing. Even minor injuries struggle to heal and become chronic wounds.
Impaired Immune Function
Elevated blood sugar impairs the immune system's ability to fight infection. Once bacteria enter a diabetic foot ulcer, the body cannot mount an effective defense, allowing infections to spread rapidly.
Why Diabetic Foot Ulcers Need Specialized Care
Diabetic foot ulcers are not ordinary wounds. They represent a medical emergency that requires immediate expert intervention:
Amputation Risk
Diabetic foot ulcers precede approximately 85% of lower-limb amputations in people with diabetes. Early, aggressive treatment is critical to limb preservation.
Rapid Infection Spread
What appears as a surface wound may harbor deep infection extending to bone. Infections can progress from cellulitis to osteomyelitis (bone infection) within days.
Silent Progression
Due to neuropathy, patients often don't feel pain even as the ulcer worsens or becomes infected, delaying treatment.
Compromised Healing
The same factors that cause diabetic ulcers also prevent healing: poor circulation, elevated blood sugar, and impaired immune response make these wounds notoriously difficult to close.
High Recurrence Rate
Even after healing, diabetic foot ulcers recur in up to 40% of patients within one year without proper prevention strategies.
Our Approach to Diabetic Foot Ulcers
Thorough Assessment and Risk Stratification Our Nurse Practitioners conduct comprehensive evaluations including:
Wound depth, size, and tissue quality assessment
Vascular evaluation (pulses, capillary refill)
Neurological assessment (protective sensation testing)
Infection screening (probing to bone, drainage assessment)
Blood sugar management review
This assessment determines wound severity and guides treatment intensity.
Contact us
Content: Every diabetic foot ulcer is a race against time. The difference between limb preservation and amputation often comes down to the speed and expertise of treatment. Our Nurse Practitioners bring specialized knowledge and proven protocols that give your diabetic patients the best chance for healing and keeping their limbs.
Contact Best Wound Care today to provide your diabetic patients with the specialized foot ulcer care that can save limbs and lives.